
Symptoms
Patients with bladder tumors may present with various symptoms, although some cases are asymptomatic, especially in the early stages. Common symptoms include:
The most common presenting symptom, characterized by blood in the urine. It can be gross (visible) or microscopic (detected through laboratory tests).
Increased frequency, urgency, painful urination (dysuria), and a sensation of incomplete bladder emptying.
Lower abdominal or pelvic pain may occur, particularly in advanced stages.
In advanced cases, weight loss, fatigue, and bone pain (if metastasized to the bones) can occur.
Risk Factors
The exact cause of bladder tumors is not always clear, but several risk factors have been identified:
Cigarette smoking is the most significant risk factor for bladder cancer, responsible for approximately 50% of cases. Carcinogenic chemicals in tobacco smoke are absorbed into the bloodstream and filtered by the kidneys into the urine, where they come into prolonged contact with the bladder lining.
Occupational exposure to certain chemicals, such as aromatic amines (found in dyes, rubber, leather, textiles, and paint products), can increase the risk of bladder tumors.
Chronic bladder inflammation, such as that caused by repeated urinary tract infections (UTIs), bladder stones, or long-term use of a urinary catheter, can predispose individuals to bladder tumors.
Previous radiation therapy to the pelvis or certain chemotherapy agents (like cyclophosphamide) can increase the risk of developing bladder cancer.
Although most bladder cancers are not inherited, having a family history of bladder cancer can increase risk.
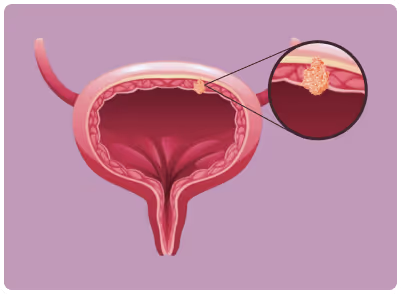
Pathophysiology
Bladder tumors develop when normal cells in the bladder lining mutate and begin to grow uncontrollably. The most common type, urothelial carcinoma, starts in the urothelial cells that line the bladder. These tumors can vary in their invasiveness:
These tumors are confined to the bladder lining (urothelium) and have not invaded the muscular bladder wall. They are generally less aggressive but have a high recurrence rate.
These tumors penetrate into the muscle layer of the bladder wall and are more likely to spread to other parts of the body (metastasize). MIBC requires more aggressive treatment due to its higher potential for progression and metastasis.
Investigations
.avif)
The diagnostic evaluation for bladder tumorstypically involves:
Detects hematuria and examines urine for abnormal cells shed by the bladder lining.
A key diagnostic procedure involving the insertion of a cystoscope (a thin, flexible tube with a camera) into the bladder through the urethra to visualize the bladder lining directly and identify any abnormal growths.
Imaging Studies: Ultrasound, computed tomography (CT) urogram, or magnetic resonance imaging (MRI) are used to assess the extent of the tumor and detect any spread to adjacent structures or lymph nodes.
Biopsy and Transurethral Resection of Bladder Tumor (TURBT): A biopsy is typically obtained during cystoscopy, and TURBT is performed to diagnose and stage the tumor by removing tissue samples for histological examination.
Management
Treatment options depend on the stage, grade, and type of bladder tumor:
Transurethral Resection of Bladder Tumor (TURBT): The primary treatment for NMIBC, involving the removal of tumors through the urethra.
Intravesical Therapy: Medications, such as Bacillus Calmette-Guérin (BCG) or mitomycin C, are directly instilled into the bladder to reduce recurrence risk.
Radical Cystectomy: Complete removal of the bladder, often with nearby organs and lymph nodes.
Radiation Therapy: May be used as a primary treatment in patients who cannot undergo surgery or as adjuvant therapy post-surgery.
Chemotherapy: Systemic chemotherapy is often used before surgery (neoadjuvant) or after surgery (adjuvant) to reduce the risk of metastasis.
Chemotherapy: Cisplatin-based regimens are commonly used.
Immunotherapy: Immune checkpoint inhibitors (e.g., pembrolizumab, atezolizumab) have been approved for advanced or metastatic bladder cancer.
Prognosis and Complications
The prognosis depends on the stage and grade of the tumor. NMIBC generally has a better prognosis, with high survival rates but frequent recurrences. MIBC and metastatic bladder cancer have a poorer prognosis, with lower survival rates due to a higher likelihood of progression and spread.
Potential complications include recurrence of the tumor, progression to a more invasive or metastatic form, urinary incontinence, and complications related to treatment (e.g., surgical complications, chemotherapy side effects).
.svg)

.svg)

.svg)
.svg)
.svg)
.svg)